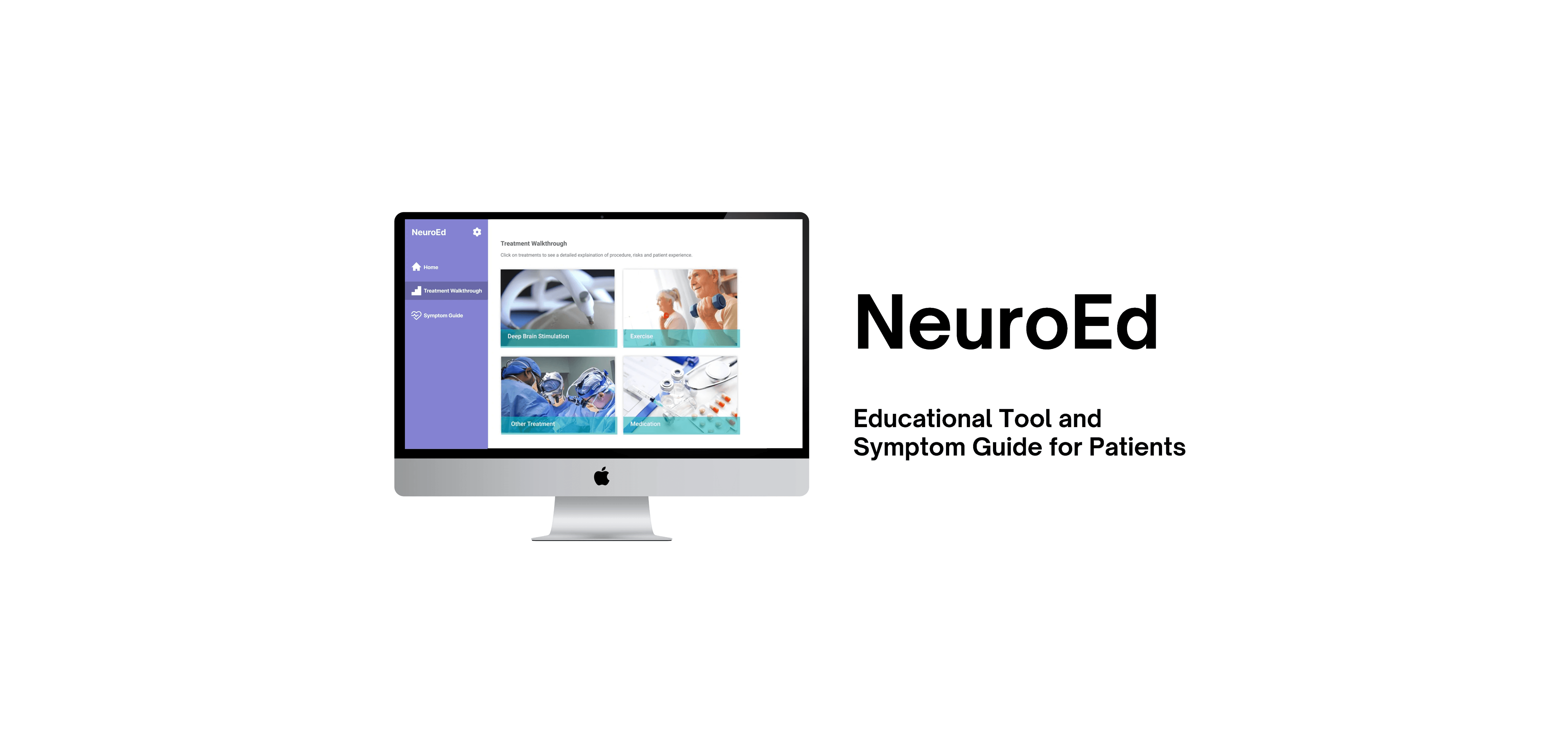
NeuroEd: Guiding Patients through Neurological Treatment and Symptom Recognition
———————————————————————————————————————————
Design Overview
———————————————————————————————————————————
NeuroEd is a website that educates patients at Rhode Island Hospital on their options for treatment based on their symptoms. The website also contains information about DBS, and a thorough overview of the Fast Track clinic, in which patients undergo a series of tests to discover whether or not they’re a good candidate for DBS.
Final Solution
———————————————————————————————————————————
Displays information about the website, instructions on using the website, and the physician care team.
————————————
——————————————
————————————
Home
Treatment Walkthrough
Symptom Guide
Contains different treatment options for patients to compare and get informed. Each treatment option includes animations and videos, along with descriptions in simple yet informative terms.
Descriptions for several neurological disorders that are suitable for DBS treatment.
Background
———————————————————————————————————————————
Deep brain stimulation (DBS) is an effective yet complex procedure for patients with Parkinson’s disease. Though informed consent is an important part of patient care, candidates for this procedure are mixed in their understanding of DBS, and struggle to understand medical terminology. The pamphlets that are given to patients contain information that can appear overwhelming and extraneous.
User Research
———————————————————————————————————————————
We first began our research by observing the neurosurgery team at Rhode Island Hospital, and figuring out which problems to solve in this space. From our initial observations, we noted that the cords in the operating room were messy, the surgical tools were difficult to locate, and maneuvering in the operating room was difficult and unsafe for everyone involved. We also conducted a contextual inquiry in the Fast Track clinic, in which patients undergo a series of tests to determine if DBS is right for them.
A typical day at the Fast Track clinic consists of the following:
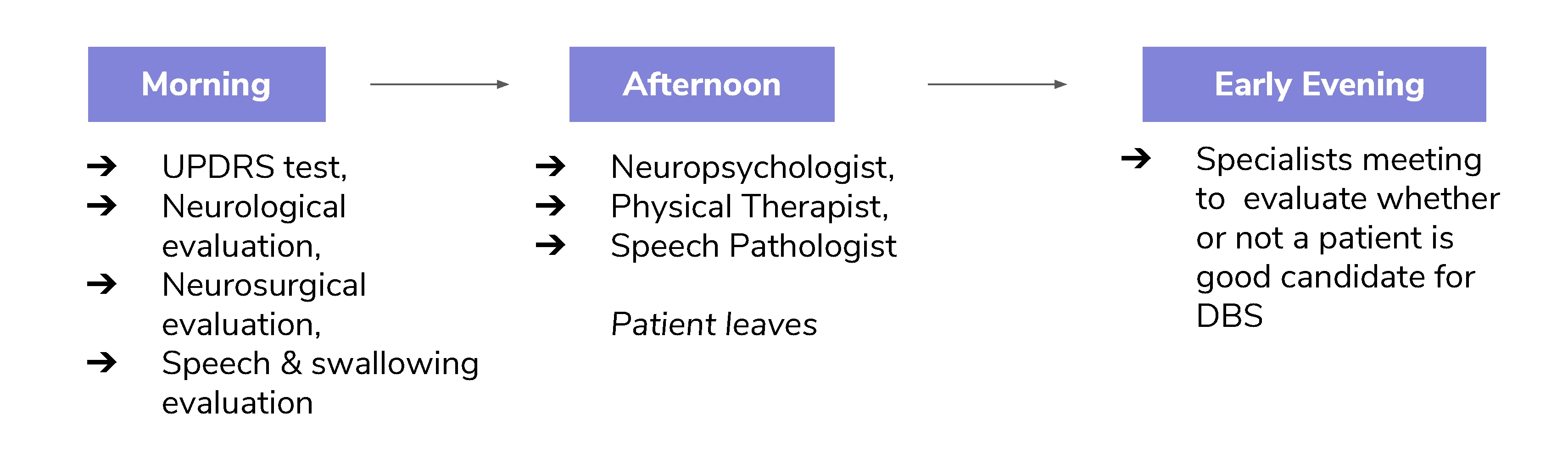
One potential problem I noticed was how long the appointment was. Patients were in the clinic from 8am to 5pm! The patients reported that they did not completely understand the medical terminology that psychologists, neurosurgeons, and physical therapists were explaining. According to the head neurosurgeon that we worked with, there isn’t enough time to go into detail about each step in the Fast Track clinic. It was clear that this could cause a problem regarding informed consent in patients.
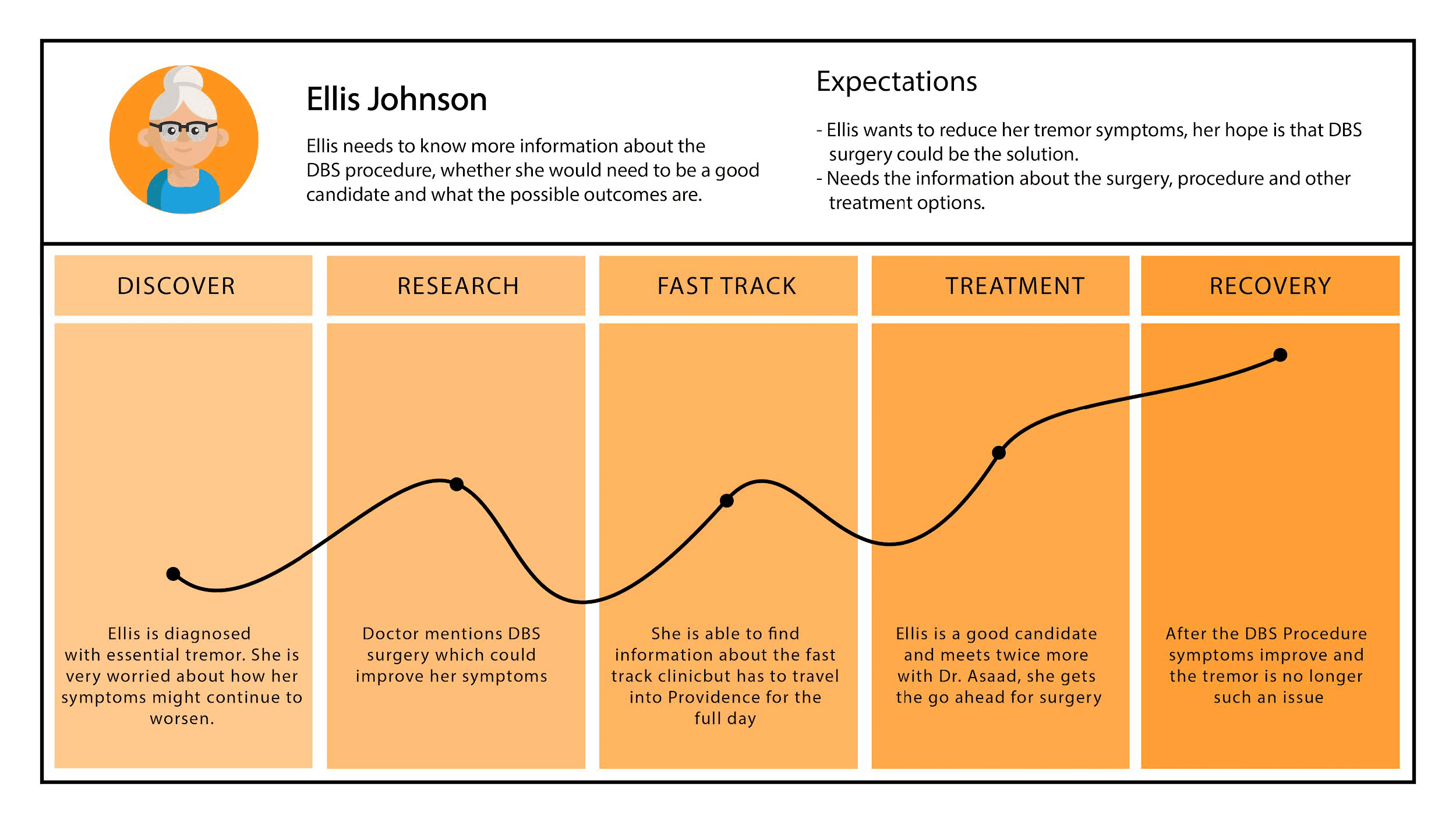
Below is an example of what one patient with a neurological disorder might experience at the Fast Track clinic, from diagnosis to recovery, at Rhode Island Hospital.
After three days or research at Rhode Island Hospital, we came up with three potential ideas for our project direction:
OR (Operating Room) Organization: Creating an efficient, clutter-free system of organizing surgical tools.
Symptom Management: A method for patients to track and manage their symptoms.
Patient Education: A website to help patients understand DBS, neurological symptoms, and types of treatments.
My team of five rated each idea, based on each of our perceptions on how promising each idea would be. We rated each idea through five criteria from low prospect to top prospect:
Feasibility: How easily this idea would be done in a hospital setting.
User Utility: How often and helpful the idea would be for users, patients and/or providers.
Cost Effectiveness: Will this idea have good value for the clinic or hospital?
Workflow Integration: Could this idea be integrated without drastically disrupting the current clinical infrastructure?
Personal Interest: How exciting is this idea to us?
Below are the results of our ratings for each of the three ideas:
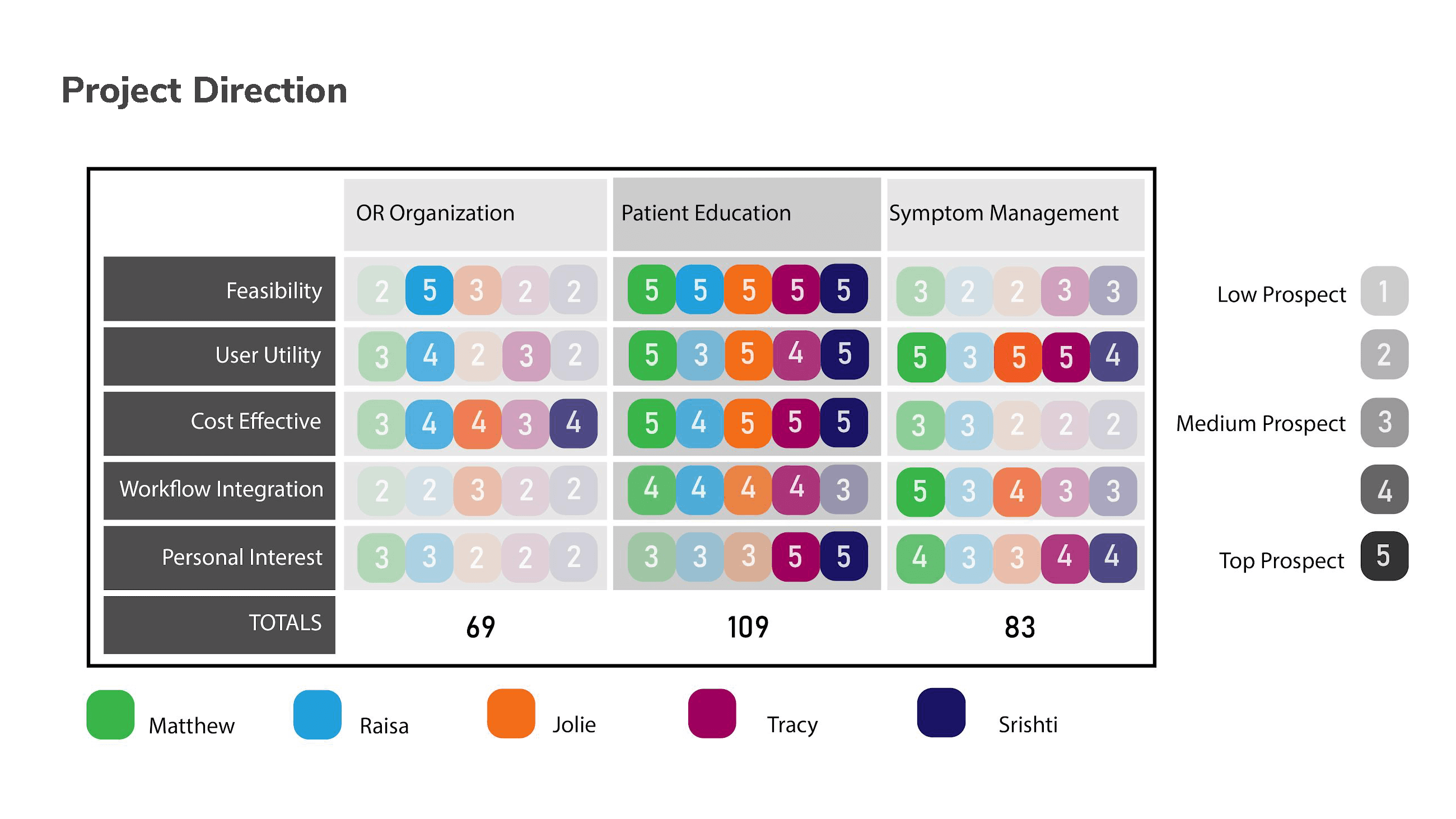
Based on our ratings, patient education was clearly the most prospective project out of the three. Through patient education, we could present detailed yet easily digestible information about DBS and to save time during pre-procedural meetings during the Fast Track clinic.
Concept Development
———————————————————————————————————————————
I and two members of the team continued to observe the Fast Track clinic to determine the kind of prototype we would create. Since the physician/patient interaction is integral to the patient’s care, and saving time during pre-procedural meetings is important, we decided to create an educational website. However, the physician who mentored our team cautioned us against offering patient-specific advice, due to liability concerns and our lack of medical training. So our website would be purely informational and educational, rather than personalized with patient data.
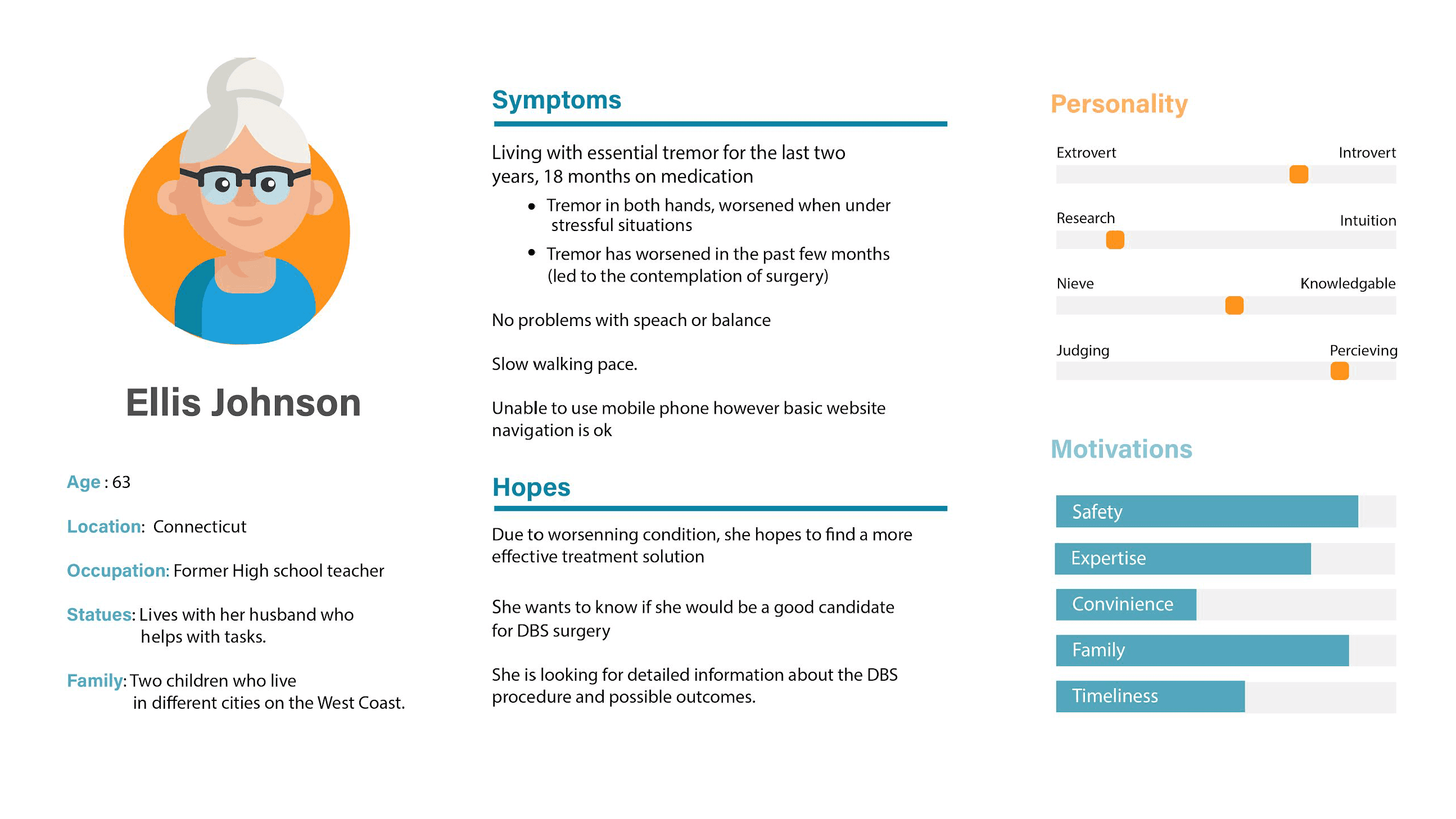
Since the average age of a Parkinson’s patient is 60 years, and all of us were in our 20s, we drafted a user persona and user journey to understand what these users might be thinking about as they're participating in the Fast Track clinic.
To understand the relationship between the physician and his patients, we created user empathy maps for both the physician and the patient and their families.
Based on these empathy maps, it is clear that there's a lot of dialogue that goes between the patient and the physician. When it comes to informed consent, there may be information that slips through the cracks, whether it involves a patient's understanding to dense terminology or a physician's concern about convering all of the information.
Putting our research together, we came up with our design goal:
For Patients: Give patients an authorized and detailed source of information, which will result in more efficient physician visits and help the patient make informed decisions.
For Physicians: Help physicians and patients stay on the same page and reduce repetition and friction in communication.
Below are the following parameters that we looked to as reference to support our design goal, as well as our design strategy moving forward:
Easy-to-digest information about DBS and neurological symptoms
Useful for doctor meetings and patients at home
An elder-friendly interface
Ideation
———————————————————————————————————————————
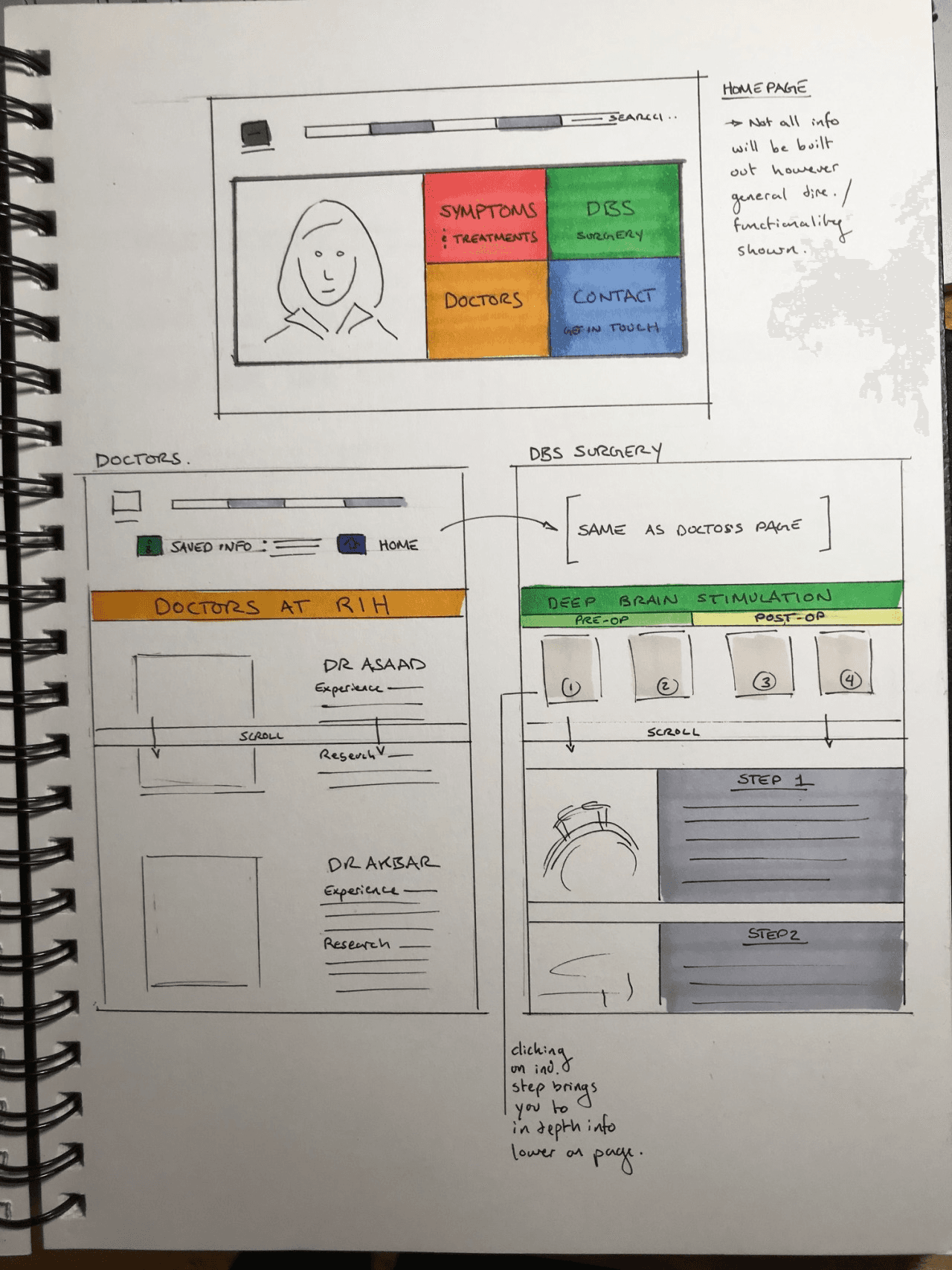
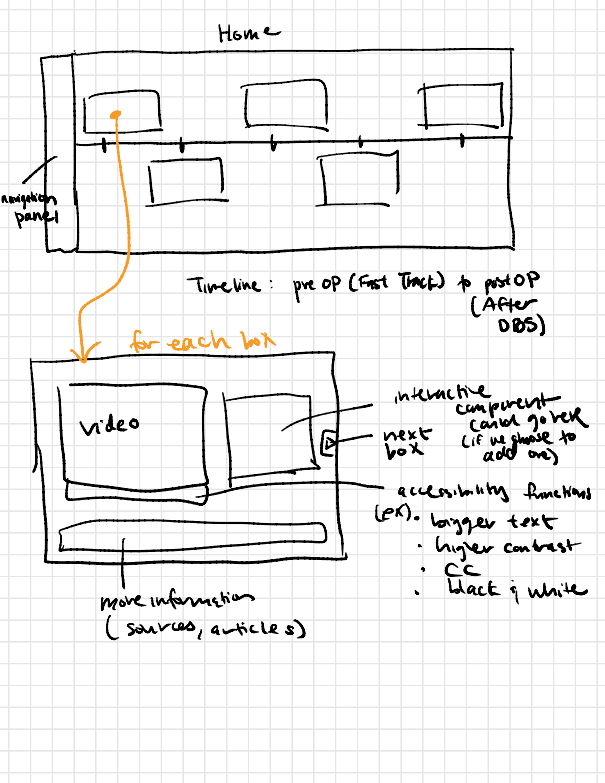
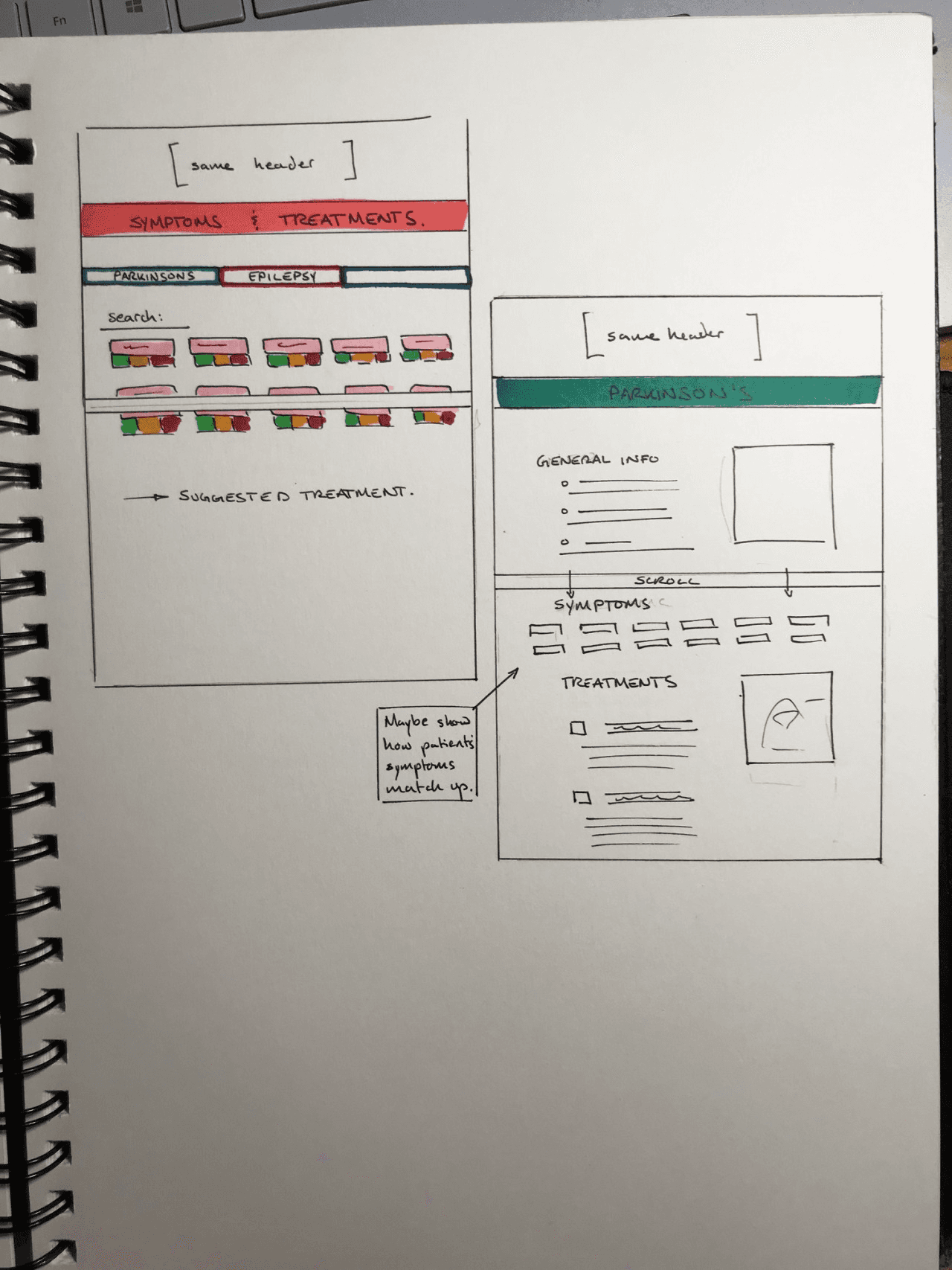
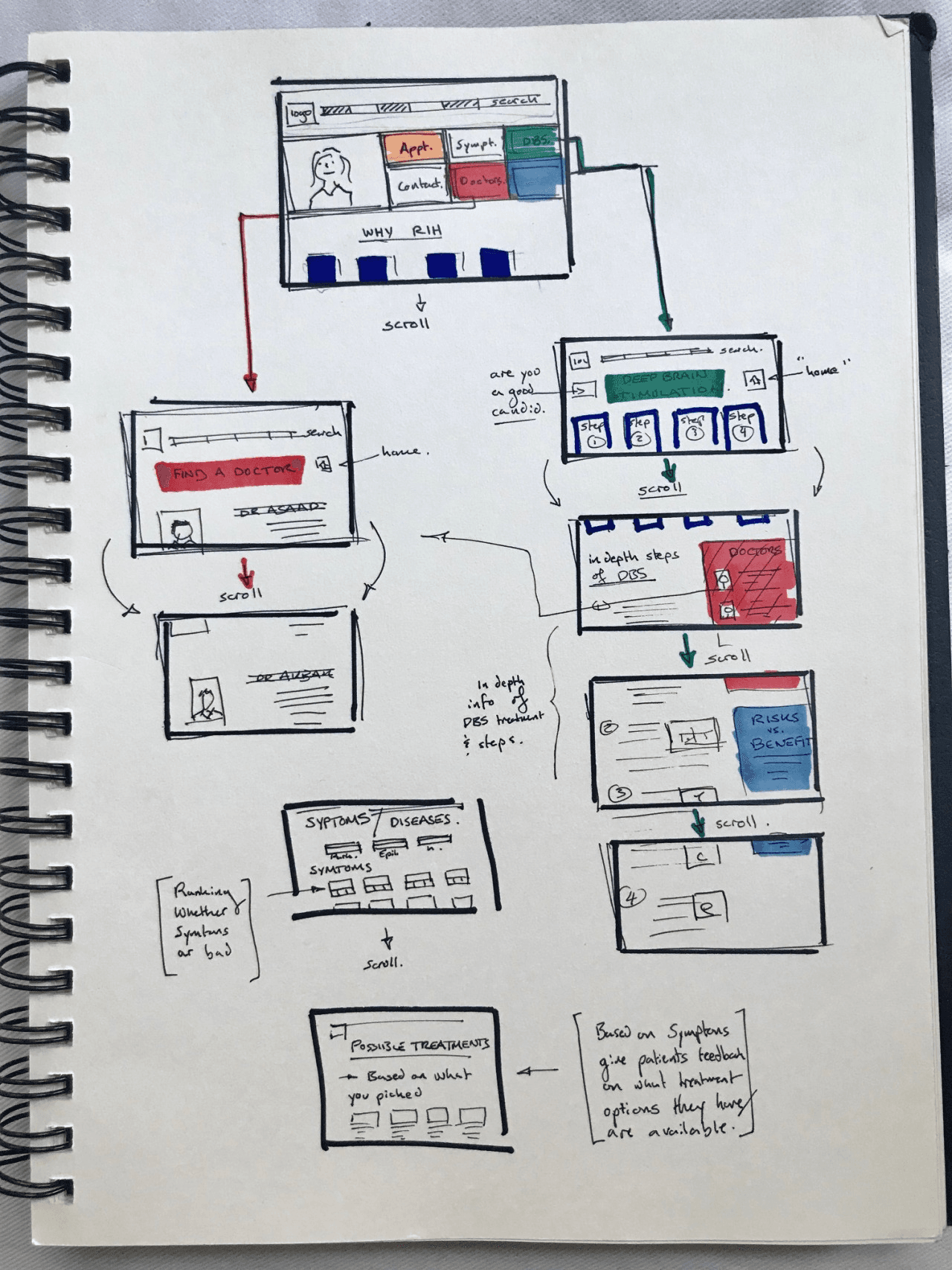
We brainstormed the architecture for the information that we should include, based on our design strategy above:
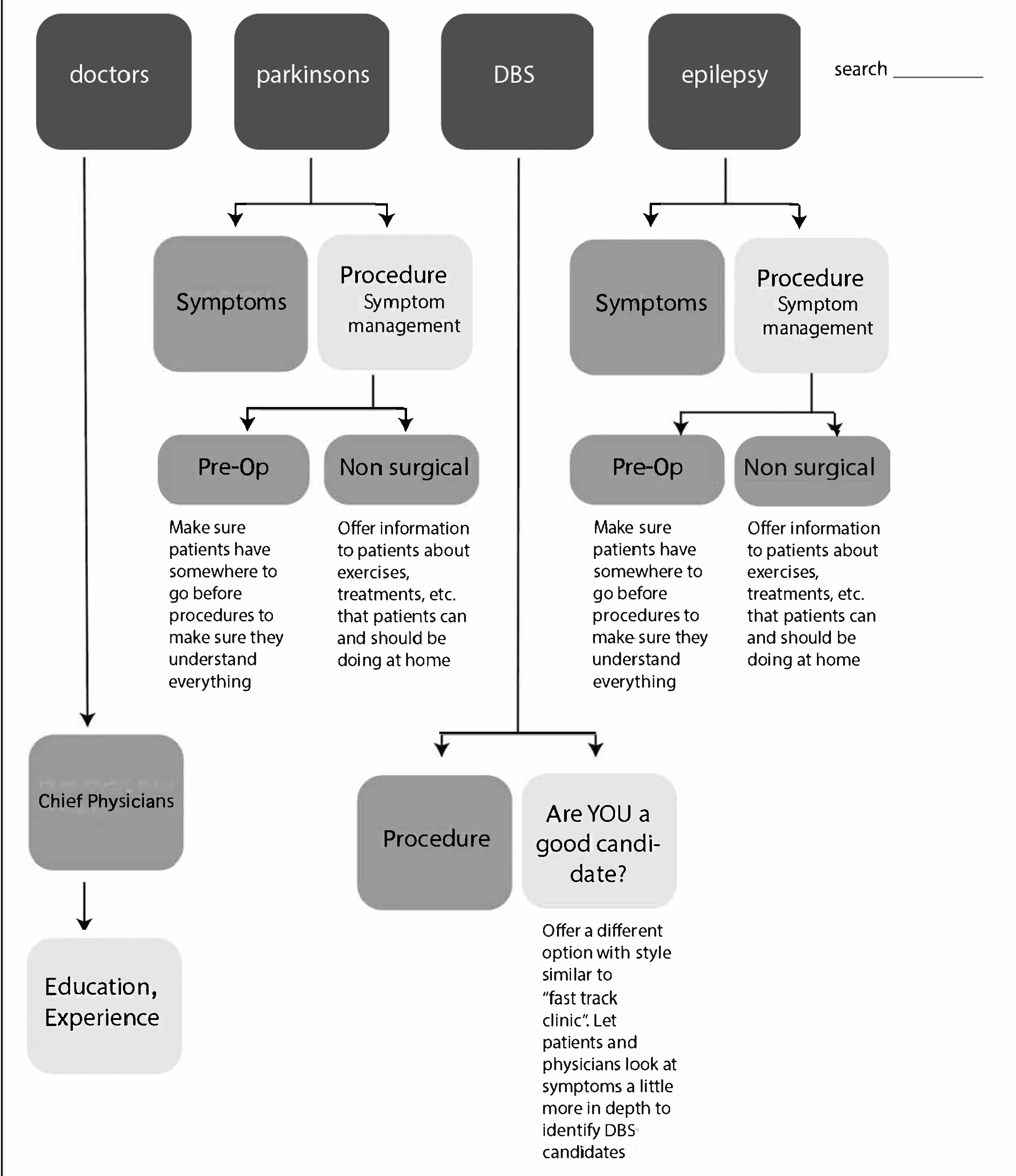
With this information, we drafted several wireframes for the website:
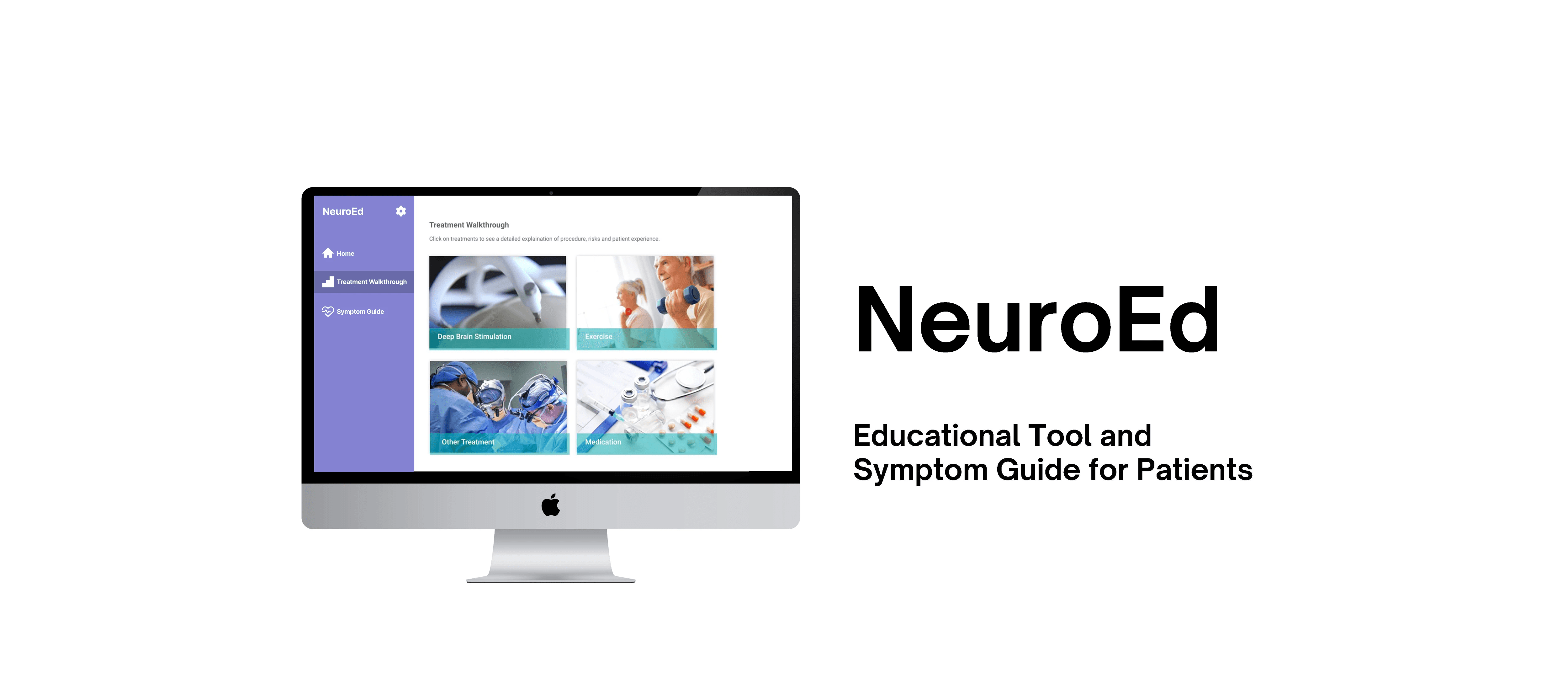
Accessibility
———————————————————————————————————————————
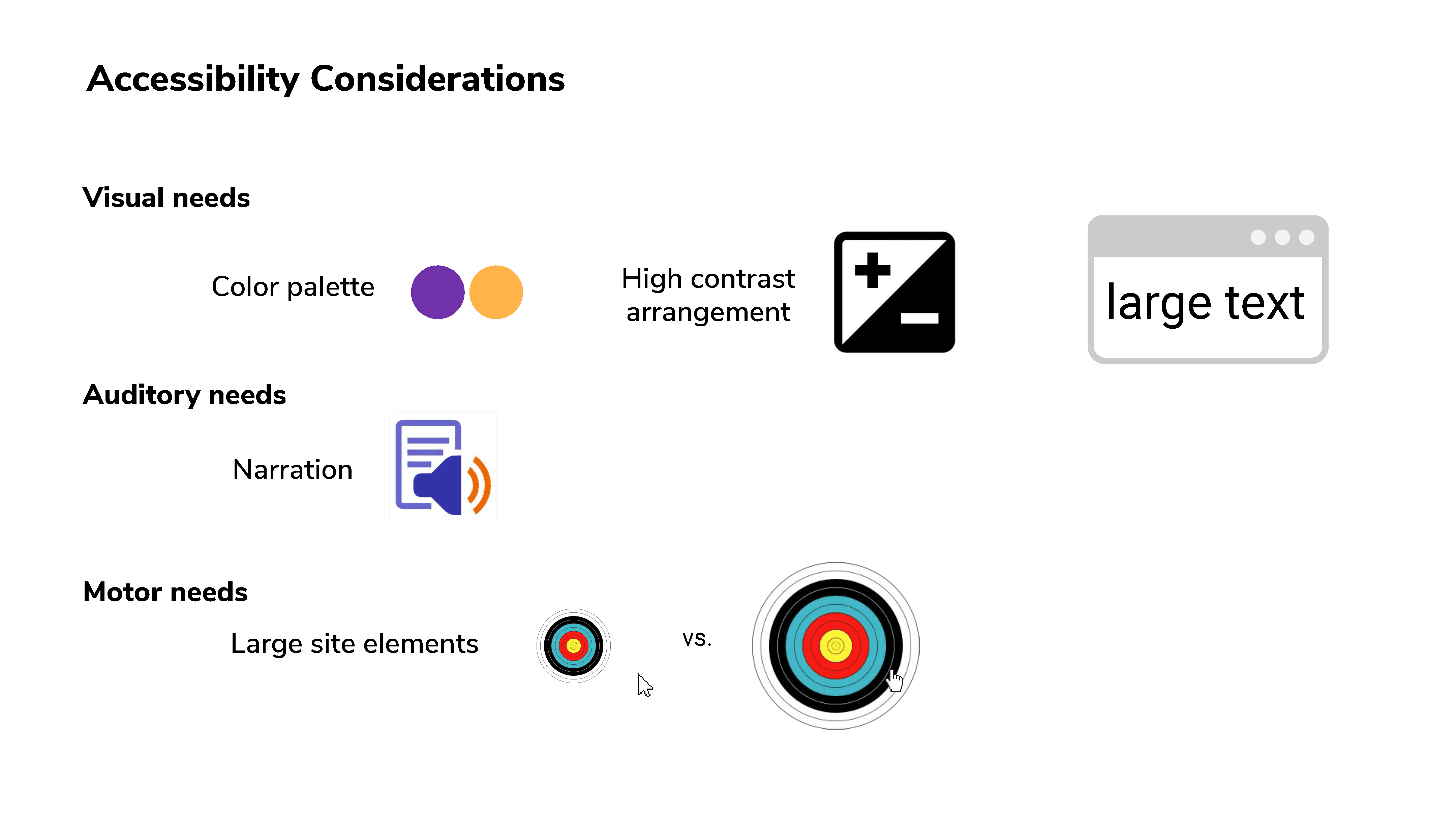
We spent a considerable amount of time looking into UI design for elderly populations and found that simple and useful designs, without extra embellishments, were the most effective. In our prototype, we made sure to include large icons and high contrast. We avoided shades of blue, which can appear faded to older populations, and we chose purples and yellows for our main color palette.
Fonts were at minimum 12-16 pt and sans serif, and buttons were at least 9.6 mm (36px) in length. Since elderly populations consistently excel in attention span, persistence, and thoroughness, long paragraphs were not something we ruled out. For those who experience vision loss, which is common, we provided text-to-voice accessibility.
Reflections
———————————————————————————————————————————
This project taught me how to design for accessibility. As the average age of patients in the Fast Track clinic was 56, it was important to create designs that effectively consider their needs. Elements such as text size, button size, and color contrast were considerations that might have crossed my mind if I were designing for a different target group. Rather than aesthetics alone, our website design was centered around the abilities of our target group, patients with neurological disorders, so we prioritized accessibility first and aesthetics second.
Additionally, working on this project challenged me to pivot from ideas that are attractive but not feasible. Our team was close to committing to solving the problem of organization in the operating room, as it provided opportunities to address issues such as safety and efficient organization. However, designing for a system that was reliably followed by the surgical team would be unnecessary, and perhaps, even harmful.
Thank you to my team, Matthew, Raisa, Srishti, and Tracy, for the hours we put into this project together. We also thank Dr. Asaad and Dr. Akbar for their medical knowledge and guidance on working with patients.